The hemorrhagic corpus luteum (HCL) is a phenomenon resulting from spontaneous bleeding into a luteal cyst post-ovulation. A rupture of HCL can lead to hemoperitoneum, characterized by abdominal pain from peritoneal irritation. Despite a broad differential diagnosis, standard management protocols are yet to be universally adopted. This review compares diagnostic and treatment modalities ranging from laparoscopic interventions to medical management, emphasizing the self-limiting nature of HCL hemorrhage.
Clinical Presentation and Diagnosis
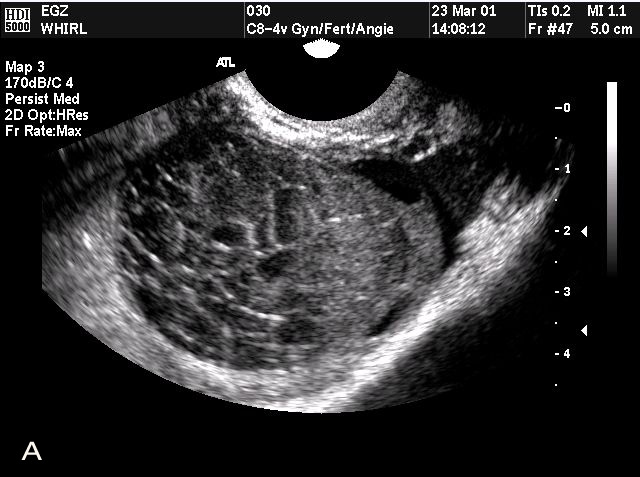
Hemorrhagic corpus luteum rupture, potentially precipitated by physical activities or trauma, presents a wide array of symptoms primarily associated with peritoneal irritation. The differential diagnosis includes ectopic pregnancy, adnexal torsion, and more, highlighting the importance of comprehensive diagnostic processes including ultrasonography and blood tests.
Strategic Approaches to Management
The management of HCL involves a dynamic assessment of clinical symptoms, hemodynamic stability, and ultrasound findings. A conservative “wait-and-see” approach is often recommended for hemodynamically stable patients, supplemented by supportive drug therapies. In contrast, persistent symptoms or hemodynamic instability may necessitate surgical intervention.
Innovations in Non-Surgical Treatment
Advancements in medical management for HCL focus on minimizing intervention-related risks and enhancing patient comfort. Strategies include the use of antifibrinolytic agents, analgesics, and fluid therapy. Importantly, for patients with coagulopathies or those on anticoagulant therapy, careful monitoring and adjustment of medications are crucial to prevent exacerbation of hemorrhage.
Surgical Interventions and Their Impact
In cases where conservative management is ineffective or in patients experiencing significant hemoperitoneum, laparoscopic surgery emerges as the preferred method. Options range from cystectomy to oophorectomy, depending on the extent of the hemorrhage and the patient’s future fertility desires. The choice of surgical technique is influenced by factors such as cyst size, patient stability, and the presence of concurrent ovarian pathology.
Stemming Recurrence in High-Risk Patients
For patients at heightened risk of HCL recurrence, especially those with bleeding disorders or undergoing anticoagulant therapy, prophylactic measures such as hormonal suppression of ovulation can be pivotal. The implementation of estro-progestinics or GnRH analogs aims to mitigate the likelihood of future episodes, emphasizing the importance of personalized treatment plans.
Comparative Analysis of Treatment Modalities
| Treatment Approach | Indications | Advantages | Limitations |
|---|---|---|---|
| Conservative Management | Hemodynamically stable patients | Minimizes intervention risks; supports natural resolution | May not be suitable for severe cases |
| Surgical Intervention | Persistent symptoms/hemodynamic instability | Immediate resolution of hemorrhage; can address underlying pathology | Invasive with associated surgical risks; potential impact on fertility |
| Drug Therapy | Supportive care for all patients | Manages pain and supports hemostasis | Does not directly resolve hemorrhage; requires careful monitoring |
Incorporating recent advancements in the understanding of HCL pathophysiology and treatment efficacy is crucial. Especially noteworthy is the potential application of insurance software development to streamline patient care protocols and enhance the delivery of tailored treatments, reflecting a multidisciplinary approach to healthcare innovation.
Key Strategies for Enhancing Patient Care in HCL Management
- Personalized Patient Monitoring: Implement tailored monitoring plans based on individual risk factors, including history of bleeding disorders or anticoagulant therapy, to swiftly identify signs of hemorrhage;
- Advancement in Diagnostic Tools: Invest in the latest ultrasound technology and training to improve the accuracy of HCL diagnosis, facilitating early and non-invasive detection;
- Interdisciplinary Team Approach: Foster collaboration between gynecologists, radiologists, and hematologists to ensure a comprehensive evaluation and management strategy for HCL;
- Patient Education: Inform patients about the signs of potential complications and the importance of prompt medical attention, enhancing self-awareness and early intervention;
- Utilization of Non-Surgical Interventions: Explore the efficacy of antifibrinolytic agents and hormonal therapies in preventing recurrence, reducing the need for invasive procedures;
- Development of Clinical Guidelines: Work towards establishing clear, evidence-based guidelines for the management of HCL, incorporating the latest research and clinical insights;
- Incorporation of Digital Health Solutions: Leverage telehealth platforms for follow-up consultations and remote monitoring, improving access to care and patient convenience.
Advancements in Hemorrhagic Corpus Luteum Research
Recent research into Hemorrhagic Corpus Luteum (HCL) has paved the way for groundbreaking advancements in the diagnosis and treatment of this condition. Innovations in imaging technology, particularly with high-resolution ultrasound and magnetic resonance imaging (MRI), have significantly enhanced the accuracy of HCL detection, enabling earlier intervention and reducing the risk of complications. Studies have also explored the molecular and hormonal underpinnings of HCL, shedding light on the role of angiogenic factors and inflammatory cytokines in the development and resolution of these cysts.
This deeper understanding has opened new avenues for pharmacological management, with research focusing on targeted therapies that address the specific pathways involved in HCL formation and bleeding. Furthermore, genetic studies have begun to identify potential predispositions to HCL, offering prospects for personalized medicine approaches in the prevention and management of this condition. These advancements not only promise improved patient outcomes but also contribute to the broader knowledge base surrounding ovarian physiology and pathology.
Future Directions in Managing Hemorrhagic Corpus Luteum
Looking forward, the management of Hemorrhagic Corpus Luteum (HCL) is poised to benefit from several promising directions in medical research and patient care strategies. One area of potential is the development of non-invasive treatments that harness the body’s natural healing mechanisms, such as promoting angiogenesis within the corpus luteum to stabilize the structure and prevent rupture. Another promising avenue is the application of artificial intelligence (AI) in diagnosing HCL, where machine learning algorithms could analyze imaging data to distinguish HCL from other ovarian cysts with a high degree of accuracy.
Additionally, the integration of personalized medicine into HCL management, where treatment decisions are informed by a patient’s genetic makeup, lifestyle, and risk factors, could significantly enhance efficacy and minimize adverse outcomes. Clinical trials are also underway to evaluate the safety and effectiveness of new pharmacological agents that could reduce the need for surgical intervention in patients with HCL. As research continues to evolve, these innovative approaches hold the potential to transform the landscape of HCL management, offering more effective, less invasive, and highly personalized treatment options for affected individuals.
Conclusion
The clinical management of hemorrhagic corpus luteum has evolved, with a greater emphasis on early diagnosis, conservative management, and patient-specific treatment strategies. Future research should focus on refining diagnostic criteria, exploring new non-surgical treatments, and developing guidelines for managing high-risk patients to prevent recurrence. Through these efforts, the medical community can improve outcomes for patients experiencing this complex gynecological condition.