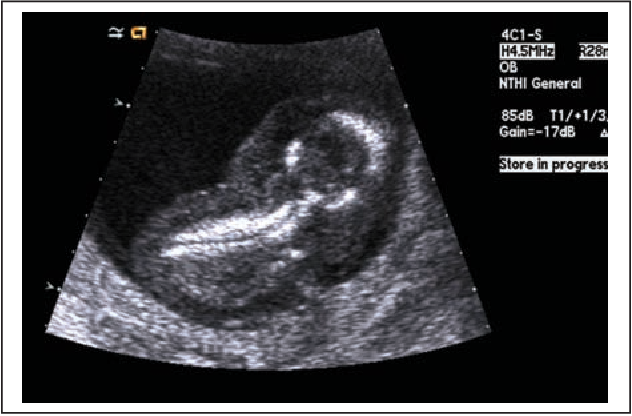
Fetal anasarca, characterized by widespread subcutaneous edema exceeding 5 mm in tissue thickness, emerges as an uncommon ultrasound discovery, often indicating advanced hydrops fetalis and the looming risk of fetal demise. This condition’s critical understanding spans its origins— immune and non-immune—to its diagnostic journey, therapeutic interventions, and prognosis.
Etiology and Diagnosis
Tracing back to Levine and Stetson’s pioneering work, the immune form of hydrops fetalis (IHF) predominantly results from Rh incompatibility between an Rh-negative mother and an Rh-positive fetus. This condition catalyzes an immune reaction leading to fetal erythroblastosis. Before the advent of Rh immunoglobulin (RhIG) prophylaxis, IHF accounted for a significant fraction of all hydrops fetalis cases. Current estimates suggest that post-RhIG intervention, IHF figures have dwindled. Diagnosis hinges on meticulous sonographic screening, underpinned by sonographer vigilance for early signs predictive of fetal anasarca.
Treatment Modalities
The management spectrum of fetal anasarca varies, with immunoglobulin therapy marking a significant downturn in adverse outcomes related to IHF. Non-immune hydrops fetalis (NHF), attributed to diverse etiologies such as cardiac anomalies, genetic disorders, and infections, presents a broader therapeutic challenge. Early detection via sonography enhances the potential for targeted interventions, including in utero treatments for arrhythmias and infections, thus improving survivability and quality of life postnatally.
Prognostic Factors
While the prognosis for fetal anasarca heavily depends on its underlying cause, the evolution of medical technology and treatments has favorably shifted mortality rates. Establishing early warning signs, thorough maternal-fetal monitoring, and the strategic application of RhIG have significantly mitigated risks associated with IHF. Conversely, the heterogeneity of NHF’s causes requires a bespoke approach to treatment, emphasizing the role of detailed fetal sonographic examinations in guiding clinical decisions.
Key Insights into Fetal Anasarca
- Diagnostic Criteria: Fetal anasarca is identified by extensive subcutaneous edema, with a tissue thickness exceeding 5 mm, pinpointed through sonography;
- Underlying Causes: It spans two categories – immune, primarily due to Rh incompatibility, and non-immune, attributed to a myriad of genetic, infectious, or anatomical abnormalities;
- Advancements in Treatment: The introduction of Rh immunoglobulin (RhIG) has dramatically decreased the incidence of immune-related hydrops fetalis;
- Importance of Early Detection: Sonographic surveillance plays a crucial role in the early identification of conditions leading to fetal anasarca, facilitating timely interventions;
- Prognostic Variability: Outcomes largely depend on the hydrops’ etiology, with some conditions allowing for in-utero treatment strategies that significantly improve survival rates.
Evolving Diagnostic Techniques for Fetal Anasarca
The diagnosis of fetal anasarca has evolved significantly with advancements in sonographic technology. Historically, the detection of such extensive fetal edema posed a challenge, often identified too late to allow for effective intervention. Modern sonography, however, enables early recognition of both immune and non-immune hydrops fetalis, a precursor to anasarca. This early detection is critical, as it opens a window for potential treatments that could mitigate or reverse the condition’s progression. Sonographers play a pivotal role in this process, where their expertise and acuity in recognizing the early signs of edema can significantly influence outcomes.
Furthermore, the detailed sonographic examination allows for a nuanced understanding of the condition’s underlying causes, which is indispensable for crafting targeted treatment plans. As diagnostic methods continue to refine, the potential for positive maternal-fetal outcomes in cases of fetal anasarca similarly expands, underscoring the importance of continuous training and development in obstetric sonography.
Treatment Innovations and Their Impact
The landscape of treating fetal anasarca has been transformed by the introduction of Rh immunoglobulin (RhIG), which effectively prevents the maternal immune response to fetal Rh-positive blood cells. This prophylactic approach has drastically reduced the occurrence of immune-related hydrops fetalis, once a common precursor to anasarca. Beyond immunological interventions, the management of non-immune hydrops has benefited from a more sophisticated understanding of fetal physiology and the development of in-utero treatments. Techniques such as fetal blood transfusions and the administration of medications directly to the fetus have shown promise in treating conditions previously deemed intractable.
The multidisciplinary approach to treatment, involving obstetricians, sonographers, and pediatric specialists, ensures a comprehensive strategy that addresses both the symptoms and underlying causes of fetal anasarca. As research progresses, new therapeutic avenues are expected to emerge, offering hope for conditions that are currently challenging to manage.
The Future of Fetal Anasarca Management
Looking ahead, the management of fetal anasarca stands at the cusp of significant advancements. The integration of genetic testing and molecular diagnostics into routine prenatal care promises to revolutionize the early identification of at-risk pregnancies. Such advancements could facilitate targeted interventions even before the physical manifestations of hydrops fetalis become apparent. Moreover, the burgeoning field of fetal surgery offers a ray of hope for correcting structural anomalies that contribute to fluid accumulation. Coupled with developments in pharmacotherapy, including the potential for gene therapy and stem cell treatments, the future holds the promise of significantly improved outcomes for affected fetuses.
However, these advancements also underscore the need for ethical considerations, particularly regarding the decision-making process for invasive interventions. As the capabilities of fetal medicine expand, so too does the imperative for clinicians, parents, and society to navigate the complex moral terrain they present.
Advancements in Prenatal Screening for Hydrops Fetalis
The field of prenatal screening has seen remarkable advancements, significantly impacting the early detection and management of hydrops fetalis, a precursor to fetal anasarca. With the advent of high-resolution ultrasound technology and the integration of advanced genetic testing, healthcare professionals can now identify risk factors for hydrops fetalis with greater accuracy and much earlier in pregnancy. This progress is crucial because the sooner a potential issue is identified, the broader the range of interventions that can be considered. For instance, the application of cell-free DNA testing in maternal blood has opened new avenues for non-invasive prenatal diagnosis, allowing for the detection of genetic anomalies that could lead to hydrops fetalis without risking fetal well-being through invasive procedures.
Additionally, the utilization of detailed ultrasound imaging enables the observation of fetal anatomy in unprecedented detail, facilitating the identification of structural anomalies or signs of fluid accumulation. These technological leaps not only offer hope for improved outcomes through early intervention but also underscore the importance of ongoing research and development in prenatal care technologies. As these screening methods continue to evolve, they promise to further enhance our ability to protect and improve the health of both mothers and their unborn children.
The Role of Multidisciplinary Care in Managing Fetal Anasarca
The management of fetal anasarca requires a comprehensive, multidisciplinary approach that brings together expertise from obstetricians, maternal-fetal medicine specialists, pediatric cardiologists, geneticists, and neonatologists, among others. This collaborative effort is pivotal in developing a cohesive treatment plan that addresses the complex needs of both the mother and fetus. The involvement of maternal-fetal medicine specialists is crucial for the ongoing monitoring of the pregnancy and the implementation of in utero therapies when possible. Pediatric cardiologists play a significant role in cases where fetal anasarca is related to cardiac anomalies, providing insights into potential interventions that can improve cardiac function before birth. Geneticists contribute to understanding the genetic underpinnings of the condition, offering guidance on prognostic factors and potential genetic therapies. Meanwhile, neonatologists prepare for the critical care needs of the neonate post-delivery, planning for interventions that may be necessary immediately after birth.
This multidisciplinary approach not only enhances the chances of a positive outcome but also ensures that the family is supported through what can be a challenging and uncertain time. The evolution of care for fetal anasarca underscores the importance of collaboration across specialties, promising continued improvements in treatment efficacy and patient support.
Conclusion
Fetal anasarca serves as a stark indicator of severe hydrops fetalis, demanding early detection, precise diagnosis, and proactive management to forestall fetal death. Advances in sonographic technology and medical treatments have progressively ameliorated outcomes, making fetal anasarca an increasingly rare sonographic finding. Ongoing research and clinical vigilance remain paramount in optimizing maternofetal outcomes in this complex condition.