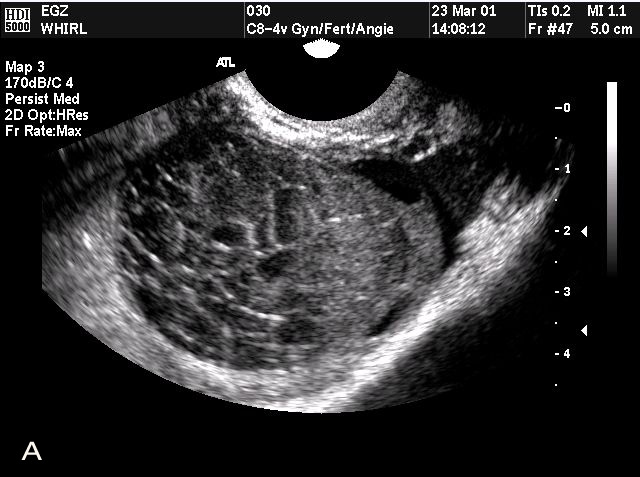
Hydrometra, a prevalent condition among postmenopausal women, encompasses the accumulation of serous fluid within the uterus. Despite its commonality, the epidemiological facets, potential harm, and predictive capacity for indicating gynecological cancers remain insufficiently defined. This study delves into these aspects, shedding light on the epidemiology of hydrometra and its association with gynecological tumors.
Methodological Approach to Studying Hydrometra
The investigation involved analyzing data from 3,903 women screened for gynecological conditions at Zhoupu Hospital, Shanghai, over the year 2021. A further detailed examination focused on 186 patients diagnosed with hydrometra through sonography, who subsequently underwent hysteroscopy and pathology evaluation, offering insights into the pathological diversity of hydrometra and its potential as a cancer predictor.
Prevalence and Risk Factors of Hydrometra
The study identified a hydrometra prevalence rate of 10.86%, surpassing other gynecological diseases. Notably, advanced age and vaginitis emerged as significant independent risk factors, highlighting the necessity for targeted monitoring in these patient groups.
Correlation Between Hydrometra and Gynecological Tumors
Among the studied cohort, a small yet notable percentage of hydrometra cases were linked to gynecological cancers. Factors such as increased body mass index, substantial hydrometra volume, and abnormal vaginal bleeding were recognized as significant predictors for the presence of gynecological tumors, underscoring the importance of vigilant screening practices.
Key Insights on Hydrometra
- Increased Prevalence: Notably higher in postmenopausal women, underscoring the need for routine screening;
- Risk Indicators: Advanced age and a history of vaginitis significantly elevate hydrometra risk.
- Predictive Value: Hydrometra volume, BMI, and abnormal vaginal bleeding are critical predictors of gynecological tumors.
Comparative Analysis: Hydrometra vs. Other Gynecological Conditions
| Condition | Prevalence Rate | Risk Factors | Association with Gynecological Tumors |
|---|---|---|---|
| Hydrometra | 10.86% | Advanced age, vaginitis | Strongly predictive of tumors |
| Endometriosis | Varies | Reproductive age, family history | Indirectly associated |
| Polycystic Ovary Syndrome (PCOS) | 5-10% | Obesity, insulin resistance | Not directly predictive of tumors |
The Epidemiological Perspective
Hydrometra, distinguished by serous fluid accumulation in the uterus, presents a notable case study in gynecological conditions. Its prevalence, especially among postmenopausal demographics, necessitates a deeper understanding and robust screening protocols. This condition, often overshadowed by more prominent diseases like endometriosis or PCOS, demands attention due to its silent progression and potential implications in predicting more severe gynecological tumors.
Clinical Implications of Hydrometra
The detection of hydrometra carries significant clinical implications, particularly in the realm of cancer prediction. The condition serves not merely as a benign accumulation but as a harbinger for potential malignancies. Early identification and management of hydrometra could pivotally influence treatment trajectories and patient prognosis, emphasizing the importance of nuanced clinical strategies and patient education in managing this condition.
Future Directions in Hydrometra Research
As the medical community continues to unravel the complexities of hydrometra, future research must focus on elucidating the molecular and physiological mechanisms underlying its development. Prospective studies could explore the potential genetic predispositions and environmental triggers contributing to hydrometra, aiming to develop preventative strategies and innovative treatments. This could significantly enhance early detection methods and refine predictive models for gynecological tumors, marking a new frontier in women’s health.
Conclusion
Hydrometra not only presents a prevalent condition among women but also serves as a crucial indicator for the potential development of endometrial and cervical cancers, particularly in individuals with significant risk factors. Recognizing and addressing hydrometra can significantly contribute to early cancer detection and improved patient outcomes, advocating for heightened awareness and diagnostic precision in clinical practice.