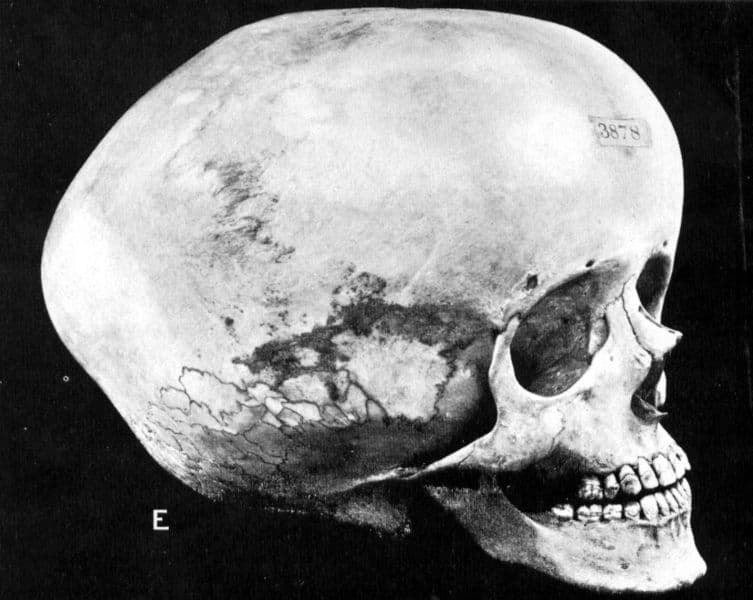
Hydrocephalus is a medical condition marked by an excessive accumulation of cerebrospinal fluid (CSF) in the ventricular system of the brain. Originating from the Greek terms for “water” (hydro) and “head” (cephalus), the condition, often referred to as “water on the brain,” is characterized by the buildup of CSF, a vital fluid that cushions the brain and spinal cord, delivers nutrients, and removes waste. This condition arises when the balance between the production and absorption of CSF is disrupted, leading to increased intracranial pressure and potential damage to brain tissues.
Origins and Types of Hydrocephalus
Hydrocephalus can manifest at any stage of life, predominantly affecting infants and the elderly. Its occurrence is relatively rare, impacting roughly one to two per 1,000 births in the United States. The etiology of hydrocephalus is varied, encompassing congenital forms present at birth, often due to genetic anomalies or fetal development issues, and acquired forms resulting from injury, infection, or disease.
The condition is classified into several types based on its cause and characteristics:
- Acquired Hydrocephalus: Develops after birth, usually due to injury or illness;
- Congenital Hydrocephalus: Present at birth, possibly related to fetal development issues or genetic factors;
- Communicating Hydrocephalus: CSF flow is unobstructed but issues with absorption or overproduction occur;
- Non-communicating (Obstructive) Hydrocephalus: A blockage hampers CSF flow between ventricles;
- Normal Pressure Hydrocephalus: Occurs in adults, characterized by dilated ventricles despite normal spinal pressure;
- Hydrocephalus Ex-vacuo: Results from brain tissue loss in adults due to degenerative diseases, leading to ventricular enlargement.
Symptoms Across Different Ages
The manifestation of hydrocephalus varies significantly across different age groups, with infants commonly exhibiting symptoms such as an unusually large head or rapid head growth, bulging fontanelles, and downward eye deviation. Children and adolescents may experience nausea, vision problems, balance issues, and developmental delays. Adults, on the other hand, might face headaches, gait disturbances, cognitive difficulties, and memory loss among other symptoms.
Diagnostic Measures for Hydrocephalus
Diagnosing hydrocephalus involves a comprehensive clinical evaluation, including a detailed patient history and physical examination, complemented by neurological assessments. Diagnostic imaging techniques such as CT scans, MRIs, and lumbar punctures are pivotal in confirming the diagnosis and guiding treatment decisions, with the involvement of neurospecialists essential for optimal management.
Therapeutic Approaches and Follow-Up Care
Treatment strategies for hydrocephalus aim to alleviate symptoms by addressing CSF accumulation, either through surgical removal of the obstruction or via the diversion of fluid using shunt systems. An alternative method, endoscopic third ventriculostomy, creates a new pathway for CSF flow. Post-operative care is crucial for monitoring neurological function and ensuring the efficacy of the treatment, with long-term follow-up necessary to manage the ongoing nature of the condition.
The Impact of Hydrocephalus on Patient Quality of Life
The implications of hydrocephalus extend beyond the physical symptoms and medical interventions, significantly impacting the quality of life of those affected. For infants and children, hydrocephalus can lead to developmental delays and challenges in learning and social integration, necessitating early intervention and support to enhance cognitive and motor skills. Adults facing this condition often encounter difficulties in daily activities, mobility, and maintaining independence, which can lead to emotional stress, anxiety, and depression. Moreover, the constant need for medical follow-up and the possibility of surgical interventions can impose financial and emotional burdens on patients and their families.
Recognizing and addressing these multifaceted challenges is crucial. Support networks, rehabilitation services, and counseling can play pivotal roles in improving the overall well-being and quality of life for individuals living with hydrocephalus, emphasizing the need for a holistic approach to patient care that considers both the physical and psychosocial aspects of the condition.
Advances in Hydrocephalus Research and Treatment
The landscape of hydrocephalus treatment and research is evolving, driven by technological advancements and a deeper understanding of the condition. Recent developments in imaging techniques and surgical tools have enhanced the precision of diagnostic assessments and the effectiveness of treatment interventions. Innovations such as programmable shunts and advances in endoscopic surgery offer more tailored and less invasive treatment options, potentially reducing the risks of complications and improving long-term outcomes.
Additionally, ongoing research into the genetic and molecular basis of hydrocephalus holds promise for the development of novel therapeutic targets and the possibility of preventive strategies. Collaborative efforts among researchers, clinicians, and patient advocacy groups are crucial for advancing our knowledge of hydrocephalus, improving patient care, and ultimately finding a cure. As the scientific community continues to unravel the complexities of this condition, there is hope for more effective treatments and a better future for those affected by hydrocephalus.
Conclusion
The prognosis for individuals with hydrocephalus is highly variable, dependent on the cause, severity of symptoms, and timeliness of treatment. While some patients experience significant improvement, others may face persistent challenges. Early diagnosis and intervention are key to optimizing outcomes, highlighting the importance of awareness and timely medical consultation for those exhibiting symptoms of hydrocephalus.