The ovaries are a pair of small, almond-shaped organs located in the pelvic cavity of the female body. They are pivotal components of the female reproductive system, with dual roles in producing oocytes (eggs) for fertilization and secreting essential hormones, such as estrogen and progesterone. These hormones regulate the menstrual cycle, contribute to the development of female secondary sexual characteristics, and support pregnancy.
Cross Sectional Anatomy
A cross section of the ovary reveals a highly organized structure divided into two main parts: the cortex and the medulla.
- Cortex: The outer layer of the ovary, known as the cortex, is where the development and maturation of oocytes occur. It is densely packed with ovarian follicles at various stages of development. Each follicle contains an oocyte surrounded by follicular cells that provide nourishment and support. The development of these follicles is a dynamic process that culminates in ovulation, the release of a mature egg into the fallopian tube;
- Medulla: The inner region, or medulla, contains blood vessels, lymph vessels, and nerves. These structures are essential for the delivery of nutrients, hormones, and oxygen to the ovarian tissues. The medulla’s rich vascular network also facilitates the removal of waste products from the ovary.
Follicular Development and Ovulation
The process of follicular development and ovulation can be observed through the changing landscape of the ovary’s cortex. Follicular development progresses through several stages:
- Primordial Follicle: The most primitive stage of follicular development, characterized by a primary oocyte surrounded by a single layer of squamous follicular cells;
- Primary Follicle: The primary oocyte enlarges, and the follicular cells transform into a multilayered structure, indicating the follicle’s preparation for further development;
- Secondary Follicle: The follicle continues to grow, and fluid-filled spaces appear between the follicular cells, eventually coalescing to form the antrum, a fluid-filled cavity that plays a crucial role in the maturation of the oocyte;
- Graafian Follicle: The fully mature follicle, ready for ovulation. The oocyte is now positioned at the edge of the follicle, surrounded by a cluster of cells known as the cumulus oophorus.
Ovulation marks the climax of follicular development, as the Graafian follicle ruptures, releasing the mature oocyte into the fallopian tube for potential fertilization.
Hormonal Regulation
The ovarian cycle, encompassing the follicular phase, ovulation, and the luteal phase, is intricately regulated by hormones. Gonadotropin-releasing hormone (GnRH) from the hypothalamus stimulates the pituitary gland to secrete follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH promotes the growth and maturation of ovarian follicles, while LH triggers ovulation and the formation of the corpus luteum, a temporary endocrine structure that secretes progesterone to prepare the uterus for pregnancy.
Pathological Considerations
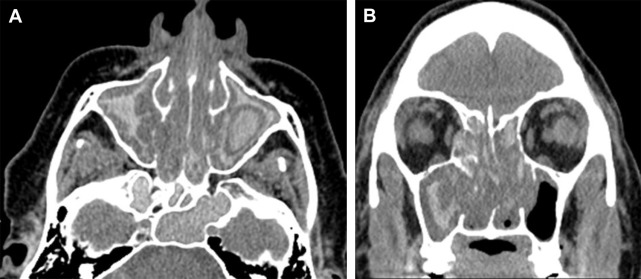
The cross section of the ovary can also reveal various pathological conditions, such as ovarian cysts, tumors, and polycystic ovary syndrome (PCOS). These conditions can disrupt the normal structure and function of the ovary, affecting fertility and overall reproductive health.
- Ovarian Cysts: Fluid-filled sacs that can develop on the ovary. While many are benign and resolve on their own, some may require medical intervention;
- Tumors: Ovarian tumors can be benign or malignant and may interfere with reproductive functions or lead to serious health concerns;
- PCOS: Characterized by the presence of multiple small cysts in the ovaries, PCOS is associated with hormonal imbalances that can affect menstrual cycles, fertility, and metabolism.
Conclusion
The cross section of the ovary is a window into the complex and dynamic world of female reproductive health. By understanding the structure and function of the ovary, along with the hormonal regulation and potential pathologies that can affect it, we gain insights into the critical role the ovaries play in fertility, hormone balance, and overall well-being. This knowledge not only advances our comprehension of human biology but also informs clinical approaches to treating reproductive health issues.
FAQs:
The ovary has two main functions: to produce oocytes (eggs) for fertilization, and to secrete hormones, primarily estrogen and progesterone, which are vital for regulating the menstrual cycle, supporting pregnancy, and developing female secondary sexual characteristics.
Ovulation occurs through a series of hormonal signals that stimulate the growth and maturation of ovarian follicles. Once a follicle matures into a Graafian follicle, a surge in luteinizing hormone (LH) triggers the follicle to rupture, releasing the mature oocyte into the fallopian tube for potential fertilization.
The cortex is the outer part of the ovary, containing ovarian follicles at various stages of development. The medulla is the inner part, consisting of blood vessels, lymph vessels, and nerves that support the ovary’s functions by delivering nutrients and removing wastes.
Ovarian cysts are fluid-filled sacs that can develop on the ovaries. While many are benign and may not cause symptoms, some can grow large, cause pain, or rupture, potentially requiring medical intervention. They can affect the normal function of the ovary, including ovulation and hormone production.
Polycystic ovary syndrome (PCOS) is a condition characterized by the presence of multiple small cysts in the ovaries, hormonal imbalances, and irregular menstrual cycles. It can lead to symptoms such as infertility, weight gain, acne, and excess hair growth. PCOS affects the ovary’s ability to produce healthy eggs and can have broader impacts on a woman’s reproductive health and metabolism.
The diagnosis of ovarian diseases involves a multi-faceted approach tailored to the individual’s symptoms and medical history. Initially, healthcare providers gather a detailed medical history and perform a thorough physical examination, focusing on the abdominal and pelvic areas to identify any irregularities. Ultrasound imaging is a cornerstone in the diagnostic process, offering a non-invasive method to visualize the ovaries and surrounding tissues, helping to identify cysts, tumors, or other abnormalities. Blood tests are critical for measuring hormone levels, including estrogen, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH), which can indicate the disease’s presence or severity. In certain cases, laparoscopy, a minimally invasive surgical procedure, allows doctors to directly observe the ovaries and other pelvic organs, providing a definitive diagnosis and sometimes offering the opportunity to treat the condition immediately. This comprehensive approach ensures accurate diagnosis and guides effective treatment plans.
Hormones play a pivotal role in the intricate process of the ovarian cycle, orchestrating every stage with precision. Follicle-stimulating hormone (FSH) initiates the cycle, stimulating the ovary to prepare an egg for release. As the follicle develops, it produces estrogen, which prepares the lining of the uterus for pregnancy. The surge of luteinizing hormone (LH) triggers ovulation, releasing the egg into the fallopian tube. Following ovulation, the ruptured follicle transforms into the corpus luteum, secreting progesterone to maintain the uterine lining for potential pregnancy. If pregnancy does not occur, the corpus luteum degenerates, leading to a decrease in hormone levels, which causes menstruation. This delicate balance of hormones not only facilitates reproduction but also influences general health, mood, and well-being, highlighting the critical role hormones play in the ovarian cycle and overall health.
Ovarian function is integral to a woman’s overall health and well-being, influencing far more than just reproductive health. It plays a central role in regulating menstrual cycles and fertility, with any disruption potentially leading to issues such as infertility or irregular menstruation. Beyond reproduction, the hormones produced by the ovaries, particularly estrogen and progesterone, have wide-reaching effects, including maintaining bone density, which can protect against osteoporosis. They also influence mood and well-being and are implicated in the health of cardiovascular and other bodily systems. Hormonal imbalances or conditions like polycystic ovary syndrome (PCOS) and ovarian insufficiency can lead to a plethora of symptoms, from weight gain and acne to more severe health implications such as increased risk of cardiovascular disease. Thus, maintaining ovarian health is crucial for preserving fertility, hormonal balance, and overall physical and mental health.